What to Expect from Ovarian Reserve Testing
- Clinic Klinic
- Jan 9
- 11 min read
You typed ovarian reserve testing into Google for a reason. Maybe you are wondering if you are running out of time to have a baby. Maybe your cycles changed, or you just got a lab result you do not fully understand.
Ovarian reserve testing can feel technical, but really it is about one simple question: "How many eggs do I likely have left, and how well might they work?"
If you are wrestling with that question right now, you are not alone at all.
The hard part is simple to identify. There is a lot of talk online, and it is easy to fall into panic or false hope. You deserve clear, grounded guidance based on real data, not fear.
Table Of Contents:
What Ovarian Reserve Actually Means
You are born with all the egg cells you will ever have. Over time, that pool shrinks, and the remaining eggs age right along with you. This overall supply and expected egg quality together are often called your ovarian reserve.
Many people think ovarian reserve is just about a number on a blood test. It is bigger than that because age, hormones, ultrasound findings, and medical history all matter. Your reserve is one piece of the larger fertility puzzle, not the entire picture.
If you have heard the phrase diminished ovarian reserve, that usually means the egg supply looks lower than expected for your age. That does not always mean you cannot get pregnant. It usually means your timeline and treatment plan should be a bit more intentional.
Understanding oocyte quantity is the first step in this journey. It reflects the number of eggs currently dormant in your ovaries. However, quantity does not always equal quality.
Even with a normal menstrual cycle, your reserve could be declining silently. That is why testing provides such critical insight. It looks under the surface of your regular monthly patterns.
Why Someone Might Consider Ovarian Reserve Testing
You might be curious about testing ovarian reserve long before you try to conceive. Or maybe you have been trying for months and want data instead of guessing. Here are common reasons people talk with a fertility clinic about it.
You are over 32 and thinking of delaying pregnancy for career or personal reasons.
You have tried to conceive for 6 to 12 months with no success.
Your cycles are getting shorter, lighter, or more irregular than before.
You are planning egg freezing or in vitro fertilization (IVF) and want realistic expectations.
You have had prior ovarian surgery, chemotherapy, or radiation.
You have a strong family history of early menopause or infertility.
You have experienced recurrent pregnancy loss.
Genetic testing factors can also change your egg supply. People with certain gene changes, such as
BRCA1 or FMR1, may see a faster drop in reserve. If that runs in your family, talking to a specialist early can be smart planning.
Your primary care provider may be the first person you ask about this. They often refer you to a specialist in reproductive medicine. This referral ensures you get a comprehensive fertility evaluation.
Types of Ovarian Reserve Testing
Doctors usually look at a mix of blood work and ultrasound for testing ovarian function. No single test can promise a baby, but together they paint a useful picture. Here are the main ones you will hear about.
1. Anti Müllerian Hormone
Anti-mullerian hormone, or AMH, is a blood test that roughly reflects the number of small growing follicles in your ovaries. These follicles each hold an immature egg. Higher AMH often suggests a larger pool, while very low AMH points to a smaller one.
AMH is a hormone produced directly by these small granulosa cells. Because of this, it gives a relatively stable reading throughout the month. An AMH level can be drawn on any day of your cycle, which makes it convenient.
But AMH is not a pass or fail score. It can vary with lab methods, birth control, and some conditions like PCOS. Doctors often remind patients that AMH predicts egg numbers much more than actual egg quality.
A very high AMH result can sometimes indicate polycystic ovarian syndrome (PCOS). This condition creates many small follicles that do not release an egg. So, a high number is not always better without context.

2. Follicle Stimulating Hormone and Estradiol
Follicle-stimulating hormone, or FSH, and estradiol are usually drawn on cycle day two or three. FSH is your brain's way of signaling the ovaries to wake up follicles. As reserve falls, the brain often pushes harder, so FSH levels climb.
Doctors often look at both FSH and estradiol together. That is because high estradiol early in the cycle can falsely calm FSH down on paper. This early estradiol rise can itself hint that the ovaries are struggling to respond.
Monitoring your FSH level helps doctors gauge how hard your body is working to ovulate. A high level suggests your system is under stress. This hormone is essentially the gas pedal for your follicle-stimulating process.
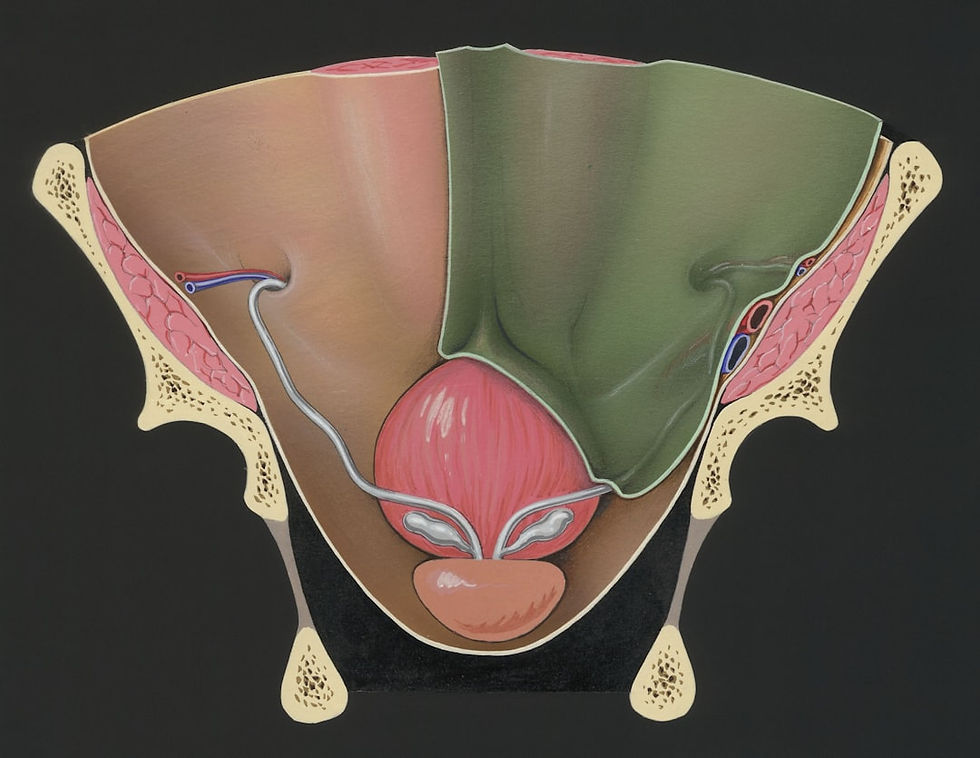
3. Antral Follicle Count
Antral follicle count, often called AFC, is an ultrasound done early in the cycle. The sonographer counts small resting follicles in each ovary, usually two to nine millimeters wide. These antral follicles represent the cohort of eggs available that month.
A higher count suggests a stronger reserve, while a low count may fit with diminished reserve. This scan can also reveal cysts, endometriosis, or structural concerns that affect treatment. Fertility clinics rely heavily on AFC to plan medication doses.
It helps avoid too weak or too strong an ovarian response. Understanding your anatomy visually helps confirm what the blood tests suggest. It is a direct look at the ovaries in real time.
4. The Clomiphene Citrate Challenge Test
While less common today, you may still hear about the clomiphene citrate challenge test. This is a dynamic test rather than a static one. It involves taking a medication called clomiphene citrate early in your cycle.
The clomiphene citrate challenge measures how well your ovaries respond to stress. You have your FSH measured on day three. Then, you take the medication for five days.
After finishing the citrate challenge, doctors measure your FSH again on day ten. A normal response shows FSH levels staying low. An elevated level suggests your reserve is diminished.
This challenge test was once the gold standard. However, the simpler citrate challenge test has largely been replaced by AMH and AFC testing. Modern clinics use it less often because AMH is easier for the patient.
What These Tests Can and Cannot Tell You
Ovarian reserve testing can be highly beneficial, but it has limitations you should be aware of. This matters so that numbers inform you, but do not control your sense of hope. Here is what you can usually learn from the results.
What testing can hint at | What testing cannot promise |
How many eggs your ovaries may release under stimulation | Exactly how many eggs do you still have in total |
Whether your reserve looks typical for your age | Whether a given cycle will end in pregnancy |
Your likely response to IVF or egg freezing medications | Egg quality in a precise way for a single egg |
Need for more prompt or adjusted fertility care | The exact age at which you will experience menopause |
Potential for ovarian dysfunction | Guarantee of a live birth |
This gap can feel frustrating at first. You are doing blood work and scans, yet there is still no crystal ball. But these tests do something valuable.
They let you make a strategy, not just wishes. They help predict response to medications. This allows for a much more personalized care plan.
How Doctors Use Ovarian Reserve Testing to Plan Care
So you do the tests, you get a panel of numbers and a scan. What actually changes next? Here is how a good clinic usually puts those results to work.
1. Timing of Trying to Conceive
If your results look strong for your age, you might have a bit more freedom around timing. That does not mean endless delay, but it can reduce urgency driven by fear. If your results hint at a faster decline, your provider may suggest starting sooner.
You might consider freezing eggs now to preserve female fertility. This locks in your current egg quality. It acts as an insurance policy for your future family building.
2. Treatment Type and Intensity
Lower reserve can shape whether simple timed intercourse or ovulation induction will be worth the months. In some cases, doctors will lean sooner toward IVF. This gives you more chances in less time.
Reserve testing prevents wasted cycles on light protocols when a stronger one is called for. Fertility treatment is an investment of time, money, and emotion. Getting the protocol right the first time matters.
Large multi-site groups often rely on standard pathways based on age and reserve data. This can mean a more consistent experience from California clinics to practices in Texas or Georgia. Wherever you go, the principles are similar.
3. Medication Dosing for IVF or Egg Freezing
Someone with a low antral follicle count may need higher doses to coax a decent number of eggs. Someone with high AMH and many follicles could respond so strongly that gentler doses are safer.
The right plan reduces risk.
It increases the odds you get a workable number of mature eggs in each cycle. Doctors carefully manage the stimulating hormone medications. This prevents complications like Ovarian Hyperstimulation Syndrome (OHSS).
4. Advanced Techniques
If egg numbers are low, clinics might use advanced lab techniques. This includes intracytoplasmic sperm injection (ICSI). With intracytoplasmic sperm injection, a single sperm is injected directly into an egg.
Sperm injection helps maximize the fertilization rate of the few eggs retrieved. This is often used when there is also a male factor issue. It makes every egg count.
5. Deciding on Egg or Embryo Banking
If your goal is to have more than one child, your team may look at how many embryos per cycle seem realistic. Reserve tests are central to that math. You might choose to do more than one retrieval now.
This effectively banks additional ovarian potential for later years. It is better to bank embryos while your eggs are younger. Trying to conceive again years later might be much harder.
Ovarian Reserve Testing and Different Life Situations
Your path and your values matter as much as your lab numbers. People come for ovarian reserve testing from all walks of life and many family visions. Here are a few common stories and how testing often fits.
You Want Kids Some Day, But Not Yet

You love your work or studies, or you haven't met a partner you want to have children with. Still, you do not want your biology making decisions behind your back. In that case, early testing gives you a rough read on your current egg supply and pace.
If you are in your late twenties or early thirties and your levels look low for your age, that is important data. You might look into freezing eggs at a clinic near you.
If your levels look very solid, you and your doctor might agree to retest in a couple of years. This allows you to focus on life now. However, regular monitoring is key to maintaining fertility health awareness.
You Are Already in Fertility Treatment
Maybe you started with basic cycles, and they just did not work. Your doctor might bring up repeating AMH or taking another look at your antral follicle count before changing gears. Updated results can explain why low-dose treatments did not work.
It can guide a shift to stronger support. At many academic clinics, ovarian reserve testing is standard. It helps build fair and realistic treatment plans.
Those programs work hard to apply the same medical insight to everyone. Whether someone is using their own eggs, a partner's eggs, or donor eggs, the data helps. Your numbers become a starting point for choices, not a judgment.
You Are Part of The LGBTQ+ Community
Maybe you are a trans man thinking about egg freezing before gender affirming hormones. Transgender care requires specific timing around fertility preservation.
Maybe you are in a lesbian couple, or you are a nonbinary person planning to carry later.
Ovarian reserve testing still matters for you. It just plugs into different pathways. You may need to pause hormones to get an accurate read on ovarian function.
Centers with dedicated queer and trans inclusive programs use reserve tests. They help with egg retrieval and choose protocols. They plan how many cycles to consider based on your biology.
You deserve a clinic that treats your gender and identity with full respect. They should also give clear, science-based options. Do not settle for less than both.
How to Read Your Results Without Spiraling
This is the hard emotional part that almost everyone underestimates. You see a low AMH or a rough phrase like diminished ovarian reserve. Your brain races ahead to worst-case stories.
So how do you stay grounded? Here are some strategies to manage the influx of information.
Do not stare at numbers in a patient portal without a real talk.
Schedule time with your fertility doctor, not just a nurse, to go through each marker.
Discuss how results fit with your age, your goals, and your partner's situation.
Bring questions written down, so stress does not make you forget.
Ask things like, based on these results, what does our best path look like over the next one to two years? How many cycles would you try before changing the plan? What outcomes do you see for patients my age with similar numbers?
Finding The Right Clinic For Ovarian Reserve Testing
The place you test and get counsel can matter just as much as the labs themselves. You want a practice that has seen thousands of cases. They should treat you like a person, not a walking set of numbers.
So what should you look for? Here is a checklist to guide your search.
Clear explanation of every test they suggest, and why.
Willingness to discuss second options, such as donor eggs, only if needed.
Reasonable wait times for new patient visits.
Strong embryology lab and high volume of IVF cases.
Experience with single parents by choice and LGBTQ families.
Transparency about insurance coverage and out-of-pocket costs.
Larger networks can be helpful. They offer choices across many states. Those networks usually have centralized lab standards and published success data.
Local independent clinics can also be excellent. Just ensure they stay current with practice guidelines from groups such as the American Society for Reproductive Medicine.
What to Do Before and After You Test
You do not have to wait for perfect lab numbers to start supporting your fertility health. Some things you can begin this month make sense at nearly any stage. They do not change your date of birth, but they help your remaining eggs work well.
Before Testing
Track your cycles for a couple of months so you can describe your pattern.
Write out your medical history and any family stories of early menopause.
Ask close relatives about breast, ovarian, or other medical history.
List any past pelvic surgeries, infections, or long-term illnesses.
Gather copies of hormone labs or ultrasounds done in the past two years.
After Testing
Give yourself at least one night before making huge decisions.
Consider a second opinion if your plan feels rushed or confusing.
Ask about simple changes like sleep or nutrition that could move the needle.
Include your partner in visits when you can.
Review the consent forms listed on the clinic's patient forms pages.
Conclusion
Hearing the phrase ovarian reserve testing can stir up a lot of fear or relief. But at its core, this testing is a tool. It gives you and your care team better sight lines on your fertility future.
It tells you how your ovaries tend to behave right now. It does not determine whether you are worthy of becoming a parent. It simply provides data to navigate the next steps.
The next move after testing is where your power lives. Do you want to try to conceive sooner, freeze eggs, change clinics, or seek more infertility treatment? You might simply choose to wait and watch.
If you are thinking about your next step right now, remember this. Your numbers matter, but your goals, support system, and values matter too. Use ovarian reserve testing as one clear voice at the table as you decide what your family-building journey should look like.
General physical. Same-day availability.



Comments