Exploring Male Fertility Testing: What You Need to Know
- Clinic Klinic
- 3d
- 9 min read
You type male fertility testing into Google for a reason. Maybe you and your partner have been trying for months and you are tired of guessing. Maybe you just want to know if everything looks okay before you start trying again.
Either way, you want straight answers about male fertility testing, without the cold medical lecture. You also want to know what is worth your money, what can be done at home, and when it is time to see a specialist.
That is what we are going to walk through here, step by step, in plain language. We will cover the entire fertility evaluation process so you know exactly what to expect.
Table Of Contents:
What Male Fertility Testing Really Looks At
Male fertility testing is less about your manliness and more about how your sperm behave in real life. The main goal is simple. Can your sperm reach and fertilize an egg under normal conditions?
This process is the core of any male fertility evaluation. It assesses your overall reproductive health to see if there are biological barriers to conception.
Most testing starts with one key lab test called a semen analysis. This initial check sets the stage for everything else.
Key Parts of a Semen Analysis
Think of a sperm analysis as a report card for your sperm. The lab checks a bunch of factors that together paint the real picture. Your healthcare provider looks at these numbers to understand your fertility potential.
Here is what they look at most often.
Parameter | What it means in real life |
Sperm concentration | The density of sperm found in a measured amount of semen |
Total sperm count | The total number of sperm present in the entire sample |
Motility | How many sperm are moving, and how well they swim forward |
Morphology | How many sperm have a normal shape and structure |
Semen volume | How much fluid do you release during one ejaculation |
pH | How acidic or basic the semen is, which affects sperm survival |
Liquefaction | How quickly the semen thins and turns to a fluid after collection |
White blood cells | Signs of inflammation or infection that could harm sperm |
Types of Male Fertility Testing
Here is where male fertility testing branches out a bit. You are not stuck with only one type of test forever. There is a kind of funnel that most doctors follow.
1. Semen analysis at a fertility lab
This is the gold standard test. You provide a sample via semen collection after a few days of no ejaculation. This is usually done by masturbation in a private room at the lab or clinic.
Some centers allow a sample from home as long as you keep it warm and deliver it fast. The lab has a strict privacy policy to handle your sample and data securely.
This test also helps check things like sperm counts after a vasectomy reversal.

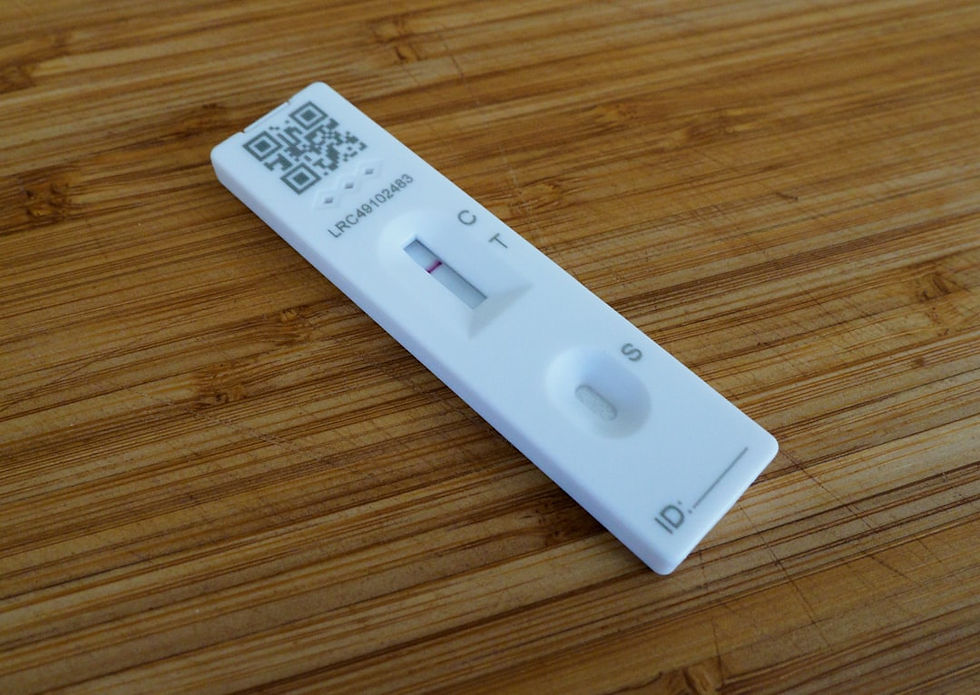
2. At home sperm tests
If the idea of walking into a clinic stresses you out, you are not alone. Home sperm tests can be a lower-pressure starting point. They are not as complete as a lab test, but they can tell you something helpful.
Products like SpermCheck Fertility measure whether your sperm count is above or below a certain level using an at-home test card. Then there are app-connected tests, such as YO Home Sperm Test, that let your smartphone camera and a small device look at moving sperm. These give a basic score for motile sperm and a report you can share with your doctor.
The point is not to replace a full semen analysis but to lower the barrier so more men actually check fertility instead of guessing. Clinic experts often view these as a useful screening tool for diagnosing male fertility issues early.
3. Hormone blood tests
If semen samples look off or there are signs like low sex drive or trouble with erections, doctors often add blood tests. These blood tests check hormone levels such as testosterone, FSH, LH, and others that control how sperm are made in the testicles. Your primary care doctor may order these initial panels to check your overall men's health status.
Think of this as checking the control system that runs sperm production, not the sperm themselves. Issues like erectile dysfunction can sometimes be linked to these same hormonal imbalances.
4. DNA and oxidative stress tests
Most guys do not jump to these right away. But for couples facing repeated miscarriage, failed IVF, or very strange semen results, doctors might order extra tests. The UCLA Men's Clinic sometimes measures sperm DNA fragmentation or levels of reactive oxygen species, called ROS.
Both of those tests show how stable the genetic material is inside the sperm and how much oxidative stress the cells are dealing with. This is also critical for cancer fertility discussions. Men undergoing treatment may need fertility preservation services before starting chemotherapy.
Male Fertility Problems Are More Common Than You Think
If you are starting to worry that any small issue on your test means the end of the story, pause for a moment. Mild to moderate male fertility problems are surprisingly common and very often fixable.
In fact, many expert groups estimate that male factors are involved in roughly one-third of infertile couples. Identifying these infertility problems early is key to achieving pregnancy.
Male Fertility Testing and Age
A lot of the public focus is on women and the ticking biological clock. You have seen the charts on female fertility decline with age everywhere. Those age patterns are real for women, but age also matters for men more than many people were told.
WebMD points out that paternal age is linked with lower sperm quality and higher risks, such as DNA damage in sperm. Sperm counts and quality can degrade over time. Maintaining a healthy lifestyle is essential for preserving fertility as you age.
What Happens During a Male Fertility Workup
You might be picturing something complicated or invasive right now. That is not how most first visits go. Most centers follow a fairly simple first-line process led by a urologist or fertility specialist who will look at your:
Health history and lifestyle to build your medical history.
Physical exam of the reproductive tract.
Semen analysis is sometimes done more than once.
Basic blood tests, often including hormones.
Your referring physician will want to check your medical records for any past surgeries or conditions.
During the physical exam, the doctor diagnoses potential issues by checking the testicles and the vas deferens. This is the tube that carries sperm, and its absence can indicate genetic conditions.
They list semen analysis, possible genetic testing, and other follow-up tools right next to treatments such as intrauterine insemination.
What Can Impact Your Male Fertility Test Results?
This is the part many guys skip over, then freak out about one bad result that could have been avoided. Small changes in your routine the days before your test really matter.
Short-term factors
Here are some common things that can throw off a single semen sample. The test involves analyzing a snapshot of your health, so timing is everything.
Having sex or ejaculating very recently, which lowers volume and count.
A recent fever or flu, since sperm production takes months.
Heavy drinking the night before the test.
Using a lubricant that is not sperm friendly during collection.
Long time between ejaculations, which can raise count but lower quality.
This is why most labs ask you to avoid ejaculation for two to seven days before testing. They are trying to get a picture that lines up with real life, not one very strange day.
Long-term lifestyle factors
Some habits wear down sperm production and quality slowly over time. These might not change your numbers in a week, but they can move them a lot over the years.
Smoking or vaping.
Heavy alcohol use or recreational drugs.
Obesity and poor metabolic health.
Sitting for very long periods with high heat around the groin.
Regular use of some anabolic steroids or certain drugs.
Recreational drugs and steroids can severely affect fertility by shutting down natural hormone production. The WebMD male fertility facts page touches on many of these, including obesity and age as key male fertility risk factors.
Part of your testing journey will likely include a hard look at a few of these areas with your doctor. Improving sperm health often starts with these lifestyle adjustments to improve fertility naturally.
Next Steps After Male Fertility Testing
You got your results back. Maybe they are pretty good with one weak area, maybe they show more clear trouble. What happens next depends on the whole picture and your specific treatment plan.
If results look normal:
This is actually very common. The semen analysis might look fine even if you have not conceived yet. In that case, your doctor may focus more on female factors or on the timing and frequency of sexual intercourse.
There might also be a conversation about subtle things such as stress, sleep, or other health issues. Understanding the menstrual cycle of your partner is critical here.
If there are mild to moderate issues:
Say count or motility is a bit low, but not zero. Many couples still conceive naturally after lifestyle changes, supplements suggested by a doctor, or a small change in timing. Sometimes doctors suggest intrauterine insemination, often called IUI.
This is where washed sperm is placed directly in the uterus at the right point in the cycle. The idea is simple. You shorten the journey and give more sperm a fair shot at reaching the egg. This is a common first-line fertility treatment.
If there are more severe findings:
Even here, it is not the end of the road. If sperm is very low, absent, or not moving at all, a male fertility specialist or reproductive urologist will usually step in. They may check for hormone problems, blockages, testicular injury, genetic factors, or health conditions such as varicocele.
Specific conditions like cystic fibrosis can cause a lack of sperm in the semen due to missing ducts.
This is often referred to as cystic fibrosis fertility issues or simply fibrosis fertility concerns. In these cases, sperm is often still produced but trapped. Treatment can include surgery, hormone therapy, sperm retrieval from the testicle, or going straight to IVF.
Doctors may use intracytoplasmic sperm injection (ICSI), where a single sperm is injected into an egg. This technique allows for fertilization even with very few sperm. For those with zero sperm production, donor sperm might be discussed.
This level of care can look overwhelming, but in vitro fertilization and advanced retrieval open doors that did not exist a generation ago.
How to Prepare for Your Male Fertility Test
It helps to treat testing as a short project, not a scary event. You can do several things in the weeks before your appointment that help you walk in with more calm and probably better data.
Get a rough timeline of your attempts so far so you can answer questions clearly.
Write down medications and supplements, including any anabolic or over-the-counter products.
Pull back on heavy drinking and smoking as much as possible.
Plan to avoid ejaculation for two to seven days before the semen test, based on the lab rules.
Ask your partner if there is anything they want you to ask during the visit.
Most doctors will remind you about abstinence timing and collection rules, but it never hurts to double-check instructions on the lab website before the day of the test. If you have a history of surgeries, infections, or injuries in the groin area, write those dates and details down too. Your care doctor can help compile this info. Being prepared helps the clinic experts get the best possible sample.
Talking About Male Fertility Testing With Your Partner
The hardest part is not always the test itself. It is the way fertility issues hit pride, hope, and relationship stress all at once. Issues like premature ejaculation or low drive can also add tension.
Here are a few simple ideas that can make the whole process easier for both of you.
Use shared language, say we are getting checked, instead of you or me.
Plan a time for a test talk instead of letting it spill out during random arguments.
Remember that fertility numbers are about biology, not worth as a person.
Look at both male fertility and female fertility by age and health, so the focus is fair.
If your results come back with some trouble spots, see them as data, not a verdict. You might also look into support groups if the stress feels too heavy. Talking with others who understand can be a huge relief.
The real value of male fertility testing is that you and your care team finally have something to work with, instead of a long line of unanswered questions.
Conclusion
Male fertility testing is not about handing your future over to a lab report. It is about using real numbers, real medical knowledge, and real conversations to make smarter choices for you and your partner. From a simple semen analysis and home kits that check your sperm count, to hormone testing and deeper DNA checks, male fertility testing gives you a clearer picture than guesswork and Google searches ever will.
You may discover that a few lifestyle changes, better timing, or a simple procedure shift the odds in your favor. Or you might learn that it is time for advanced help like IUI or IVF, with doctors who look at both partners as a team.
Either way, knowing beats worrying. Your next step is small. Book the test, ask the hard questions, and treat the numbers you get back as a starting line, not the end of the story.
General physical. Same-day availability.



Comments